
The Savior For a Slow Heartbeat! Introduction to the Functions and Types of Heart Pacemaker
Arrhythmia is a symptom that many patients with heart disease may experience. In addition to treatment with anti-arrhythmia drugs, a pacemaker can also be used to keep the heart beating regularly. This article will take you to understand how heart rhythm regulators work, and introduce their types, applicable groups and related precautions.
How does a heart pacemaker work?
The generation of “heart rhythm” relies on the sinus node (SA node, also known as the rhythm point) to send electrical impulses to stimulate the heart muscles to produce heartbeats. When the SA node no longer sends electrical impulses normally, or the electrical signal encounters obstacles in the conduction , arrhythmia or bradycardia (Bradycardia) may occur.
A heart rhythm regulator, also known as a cardiac pacemaker, is a small instrument implanted in the chest or abdomen. It can detect the user’s heart rate and deliver an electric shock when the heart rhythm is abnormal or too slow to restore the heart rate to normal. The pacemaker will intervene at the appropriate time to replace the sinoatrial node, send or stabilize current signals, and return the heart rhythm to normal. When arrhythmias occur, patients may experience fatigue, difficulty breathing, or even fainting, which can all be improved by a pacemaker.
In addition, the pacemaker is also different from the Implantable Cardioverter Defibrillator (ICD): the pacemaker is mainly used to adjust bradycardia and cardiac resynchronization therapy (CRT), while Defibrillators are generally suitable for tachycardia and asystole.
Types of heart pacemaker
Heart rhythm regulators can be divided into temporary and permanent. This article mainly introduces permanent heart rhythm regulators. Most regulators come with wires, batteries, and electronic chips, but “wireless” heart rate regulators are now available. Some new heart rhythm regulators can also detect blood pressure and respiratory rate, and adjust to a suitable heart rate based on the body’s activity. But in terms of basic functions, they can generally be divided into the following three types:
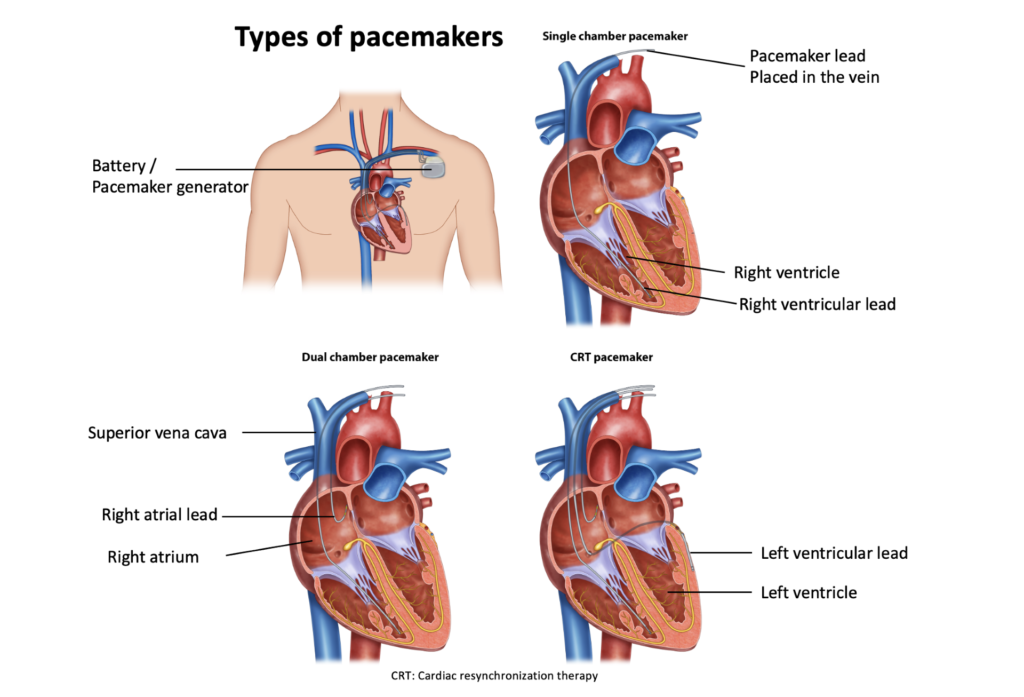
- Single-chamber pacemaker: Only one lead is connected to the right ventricle or right atrium, which stimulates the heart with electrical discharges when necessary.
- Dual-chamber pacemaker: Each has a wire connecting the right ventricle and the right atrium. When necessary, it will discharge to stimulate and control or coordinate the contraction frequency between the two chambers.
- Biventricular pacemaker (CRT pacemaker): Also known as cardiac resynchronization therapy, it is usually used in heart failure patients with abnormal heart electrical activity. The wires of this device connect the right atrium and left and right ventricles, stimulating them to beat synchronously and enhancing the heart’s ability to contract to pump. produce enough blood.
Who needs a pacemaker?
Generally speaking, patients with bradycardia or atrioventricular block (AVB) require a pacemaker to improve their heart condition. The following are possible factors that may cause these symptoms:
- Sick sinus syndrome: Aging or heart disease may damage the function of the sinus node, causing symptoms such as slower heart rate, longer intervals, or fast and slow heartbeats.
- Drugs: Some heart disease drugs, such as beta-blockers (β-Blockers), may cause bradycardia as a side effect.
- Long QT syndrome
- Fainting or other symptoms of slow heartbeat
Pre-installation diagnostics
Before installing a pacemaker, the physician may learn the type and cause of the arrhythmia through the following methods:
- Electrocardiography, ECG or EKG
- Holter monitoring
- Echocardiography
- Stress test
Risks of Heart Rhythm Regulator Use
The development of cardiac rhythm regulators is well established and, in most cases, the chance of serious complications is minimal. The following are possible risks for heart rhythm regulator users:
- Implantable pacemaker infection
- Swelling, bruising, bleeding, or nerve damage at the site where the pacemaker is installed
- Collapse of the lung (Atelectasis)












