
What Should I Do if I Have an Irregular Heartbeat? Irregular Heartbeat Symptoms, Causes, and Treatments
What is arrhythmia?
The heartbeat rate of a normal adult at rest is 60 to 100 beats per minute, and most people are between 60 and 80 beats. Arrhythmia refers to a condition in which the heart beats too slowly, too fast, or irregularly. When an arrhythmia occurs, you may feel your heart pounding loudly (palpitations) or your heart racing rapidly.
Although most arrhythmias are benign, serious arrhythmias can still be dangerous. The heart may be unable to transport blood throughout the body, resulting in organ damage or failure to function, which can even be life-threatening.
Symptoms of irregular heartbeat
The following are common symptoms of arrhythmia:
- A throbbing sensation in the chest or neck
- Rapid heartbeat or conscious heart pounding
- Slow heartbeat
- Chest pain
- Out of breath
- Lightheadedness or dizziness
- Sweating
- Fainting or about to faint
- Sudden cardiac arrest
This does not list all possible symptoms. If you have any concerns, please consult your physician.
When should I seek medical examination?
If you have any of the above symptoms or signs, please contact your physician. Everyone’s physical condition is different. Only after discussing with your doctor can you get the most appropriate care.
Causes of arrhythmia
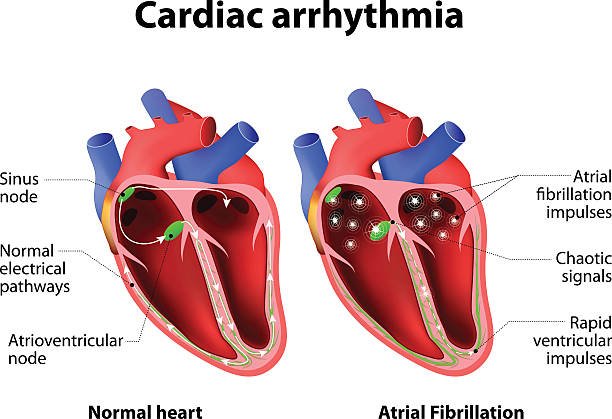
In a healthy heart, the heartbeat signal originates from the sinus node (SA node) in the right atrium, stimulating the atrium to contract and allowing blood to flow into the ventricle. The signal is then conducted to the atrioventricular node (AV node), and then Through specific conduction pathways, the ventricles are allowed to contract in order to send blood to the lungs or throughout the body.
Arrhythmia may occur when the electrical signals that control the heartbeat are delayed or blocked, the sinoatrial node does not function properly, or the electrical signals cannot be transmitted to the heart normally.
In addition, if electrical signals are generated in parts of the heart that are not supposed to generate signals, disrupting the signal transmission of special nerve cells and destroying the normal heartbeat frequency, it may also cause arrhythmia.
Common causes of arrhythmias include:
- Gene
- smoking
- pressure
- substance abuse
- Diabetes (recommended reading: Understanding Diabetes: Causes, Symptoms, Diagnosis, Prevention)
- Certain medications or nutritional supplements
- heart disease
- Drinking too much alcohol or consuming too much caffeine
- Structural changes in the heart caused by cardiomyopathy
- Sleep apnea
- High blood pressure
- Scar tissue in the heart muscle from a past heart attack (myocardial infarction)
- Hypothyroidism
- Hyperthyroidism
- Coronary artery disease (also known as ischemic heart disease)
What are the risk factors for arrhythmia?
Many factors can cause arrhythmia, such as:
- Thyroid problems.
- High blood pressure:
Increases the risk of coronary heart disease, which may cause the walls of the left ventricle to become stiff and thick, affecting the flow of electrical impulses through the heart. - Diabetes:
If diabetes is not well controlled, the risk of coronary heart disease and hypertension will be greatly increased. - Drinking too much alcohol:
Can affect the heart’s electrical impulses and increase the chance of developing atrial fibrillation. - Caffeine or nicotine:
Caffeine, nicotine, and other stimulants can speed up the heart and cause more serious arrhythmias. Some illegal drugs, such as amphetamines and cocaine, can severely affect the heart’s rhythm, leading to sudden death from ventricular fibrillation. - Electrolyte imbalance:
Electrolytes are important to the body. Potassium, sodium, calcium and magnesium help trigger and conduct electrical impulses in the heart. Electrolyte imbalance can affect the heart and cause irregular heartbeats. - Medications and nutritional supplements:
Some over-the-counter cough and cold medicines, as well as certain prescription drugs, may cause irregular heartbeats. - A history of cardiovascular disease or cardiac surgery:
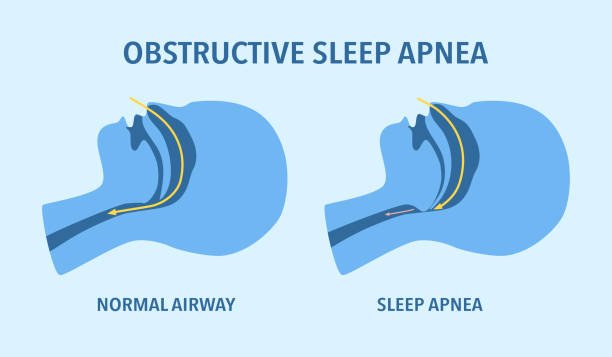
such as myocardial infarction, heart failure, heart valve insufficiency, congenital heart disease, etc. - Obstructive Sleep Apnea (OSA):
Increases the risk of bradycardia, atrial fibrillation, and other irregular heartbeats.
2 major types of arrhythmia
Generally speaking, arrhythmias are divided into tachycardia (Tachycardia) and bradycardia (Bradycardia) according to their structure, location, and beating frequency. Other irregular heart rhythms include premature contraction of the atria and ventricles.
Tachycardia
Tachycardia is also known as tachycardia, fast heartbeat, and frequent pulse. Tachycardia is defined as a resting heart rate (the heart rate during an awake, quiet state) of more than 100 beats per minute. The following are categories of tachycardia:
- Atrial fibrillation
- Atrial flutter
- Supraventricular tachycardia (also known as paroxysmal supraventricular tachycardia)
- Wolff-Parkinson-White syndrome
- Ventricular tachycardia
- Ventricular fibrillation
- Long QT syndrome
- Sinus tachycardia
Bradycardia
Bradycardia is also known as bradycardia, bradycardia, slow pulse, and bradycardia. Bradycardia is defined as a resting heart rate (the rate of heartbeat during an awake, quiet state) of less than 60 beats per minute. It is important to note that exercise, frequent exercise, or deep relaxation may also have a lower resting rate.
- Bradycardia
- Atrioventricular block
- Sinus bradycardia
Diagnostic methods for cardiac arrhythmia
Initially, your doctor will take a medical history and order tests to determine the cause of the arrhythmia, such as heart disease or thyroid problems. In some cases, your doctor may recommend heart monitoring tests, including:
- Electrocardiogram (ECG for short):
An electrocardiogram records the electrophysiological activity of the heart in units of time. - Holter 24-hour continuous electrocardiogram (Holter monitor):
This is a small, portable electrocardiogram device that can be worn throughout the day or longer to record heart activity. - Cardiac event monitor (Event monitor):
Cardiac event monitor (Event monitor): In order to diagnose sporadic episodes of arrhythmia, the patient presses the switch as soon as an episode occurs. In this way, the abnormal heartbeat can be recorded. It is suitable for cases where there are no episodes of arrhythmia every day, or if the 24-hour electrocardiogram does not detect it. - Echocardiogram:
Evaluates and tracks the structure, function, and movement of the patient’s heart and great blood vessels. - Implantable loop recorder:
A device implanted under the skin on the chest to monitor unusual heartbeats.

If the doctor does not find arrhythmia during the above tests, he may induce arrhythmia through other tests to understand the actual situation. The following are possible ways:
- Stress test:
An exercise tolerance test. Problems are more likely to be diagnosed when your heart is working hard and beating fast, so a stress test will ask you to do some exercise to get your heart beating faster. If you are unable to complete the exercise, your doctor may prescribe medication to stimulate your heart to perform as well as during exercise. - Tilt table test:
Your doctor may recommend this test if you have ever fainted. You will start by lying on a bed, then adjust the angle of the bed to make it upright. The change in position may make you feel uncomfortable (for example: dizziness, nausea, night sweats, blurred vision, and other symptoms similar to those that occur during normal attacks). Throughout the test, medical staff will observe symptoms, including heart rate, EKG readings, and blood pressure. - Electrophysiologic testing and mapping (EPS):
Using cardiac catheter technology, multiple electrode catheters are placed into the heart to record the conduction path and time of cardiac electrical waves and induce usual arrhythmias to help doctors identify The origin of the arrhythmia determines treatment.
In addition, the cardiologist may use electrode stimulation to trigger the heartbeat to see if it can induce or slow down the arrhythmia. This method allows doctors to find the origin of the arrhythmia and its possible causes.
Treatment for arrhythmia
There are many types of arrhythmias. Doctors will choose the treatment method suitable for the patient based on professional judgment through electrocardiogram, physical examination, etc. The main ones are as follows:
- Vagal maneuvers:
Stimulate the vagus nerve through specific methods (such as ice water facial application method, breath-holding method, coughing method, vomiting method, neck pressing method, inversion method, etc.) to slow down the heartbeat and relieve supraventricular dysfunction. Tachycardia. However, not all arrhythmias can be relieved in this way. - Cardioversion:
If you have atrial fibrillation, your doctor may choose cardiac rectification, which is a medical method that uses electric shock or drugs to convert an abnormal heart rate into a normal heart rate. Synchronous shock heart rate adjustment is a method of using a specific dose of electric shock at a specific time in the heart rhythm to correct the abnormal activity of the heart’s electrical conduction system. Defibrillation uses a specific dose of electric current to shock the heart at any time. This is the most effective method to rescue patients with cardiac arrest caused by ventricular fibrillation and pulseless ventricular tachycardia. - Catheter ablation:
Can block abnormal circuit conduction pathways that cause arrhythmia. During the electrocautery process, a special electrocautery catheter will be inserted (through the groin, hands, chest, and neck) to the area where the abnormal heart activity occurs. Heat, extreme cold, or radiant energy is generated through the front end of the catheter, causing abnormal conduction pathways to produce resistance. - Medications:
For many types of tachycardia, doctors may prescribe medications to control the heart rate. Generally, it can be divided into four types: Sodium channel blocker, Beta blocker, Potassium channel blocker, and Calcium channel blocker.
It is very important to take your medication exactly as directed by your doctor to reduce the risk of other complications. If you have atrial fibrillation, your doctor may prescribe blood-thinning medications to prevent blood clots from forming.
Implantable devices
Treatment for arrhythmia may also include implantable devices:
- Pacemaker:
It is an implantable device that can help patients control abnormal heartbeats. The device involves minor surgery, implanting the device into the skin near the collarbone, and using insulated wires to extend and permanently secure the device to the heart. The regulator uses electric shocks to continuously and regularly stimulate the heart muscles to maintain the heart’s continuous beating. If an abnormal heart rate is detected, it will also send out electrical pulses to stimulate the heart. - Implantable cardioverter defibrillator (ICD):
If you have ventricular tachycardia or ventricular fibrillation, or have had a cardiac arrest or are in a high-risk group for cardiac arrest, your doctor may recommend this instrument. Implantable defibrillators are very similar to the aforementioned cardiac regulators. They are implanted near the collarbone and connected to the heart through one or more electrode leads. The biggest difference between them is that ICD can send out electric current to “defibrillate”. When the heart suffers from severe arrhythmia, it can be “restarted” through defibrillation to restore the heart rhythm to normal. In addition, the ICD can also continuously monitor the heart rate. If an abnormal heart rate is found, it can also send out an electric current to maintain the regularity of the heart rhythm. Therefore, the ICD can also be said to be a heart rhythm regulator with more functions.

Surgery for arrhythmia
In some cases, your doctor may recommend surgery:
Maze procedure:
During the operation, the surgeon makes multiple barriers in the right atrium and left atrium, so that the electrical activity is limited to the atrium barrier, blocking the electrical circuit and limiting the occurrence of atrial fibrillation. Because the electrical current cannot pass through scar tissue, it can effectively interfere with stray electrical impulses that cause certain types of cardiac arrhythmias. This surgery is very effective for both paroxysmal and persistent atrial fibrillation. However, due to the long operation time and high risks, it is only suitable for patients who have poor response to drug and cautery treatment, or for other structures. Sexual problems, patients with atrial fibrillation requiring cardiac surgery.
Coronary bypass surgery:
If you have severe coronary heart disease, in addition to an irregular heartbeat, your doctor may perform coronary artery bypass surgery to improve blood flow to the heart.
Lifestyle adjustments and home therapies to improve arrhythmia
Arrhythmia may be a complication of coronary heart disease or other heart diseases. Therefore, improving your lifestyle and bad habits can reduce the risk of arrhythmia. You can take the following approaches:
- A heart-healthy diet (e.g., DASH diet, Mediterranean diet).
- Exercise regularly (30 minutes a day).
- Quit smoking.
- Avoid drinking too much alcohol.
- Be aware of the effects of your medications. Some medications may speed up or slow down your heartbeat.
In addition, you can reduce stress and reduce the risk of stress-related arrhythmias by:
- Yoga
- meditation
- relaxation techniques
In addition, some studies show that acupuncture may help reduce the occurrence of arrhythmias, but further confirmation is needed. Although there are no studies to confirm this, some people believe that omega-3 fatty acids may be helpful in treating and preventing cardiac arrhythmias.












