
Don’t Ignore Numbness and Chills in Your Feet! 7 Major Risk Factors, Causes and Prevention of Peripheral Arterial Occlusive Disease
Autumn and winter are the seasons for cardiovascular diseases. In addition to coronary heart disease, which can easily lead to sudden death, such as angina pectoris and myocardial infarction, another invisible killer is peripheral arterial occlusion disease, which is often asymptomatic in the early stage or only involves numbness, coldness or indirect pain in the feet. Sexual claudication is easily misdiagnosed as other diseases; studies have shown that even if patients with peripheral artery occlusion do not have myocardial infarction or ischemic stroke, the mortality rate is similar to the cardiovascular mortality rate of patients with heart and cerebrovascular diseases; this article will guide you Understand, what exactly is peripheral arterial occlusive disease? What are its symptoms, risk factors and prevention methods?
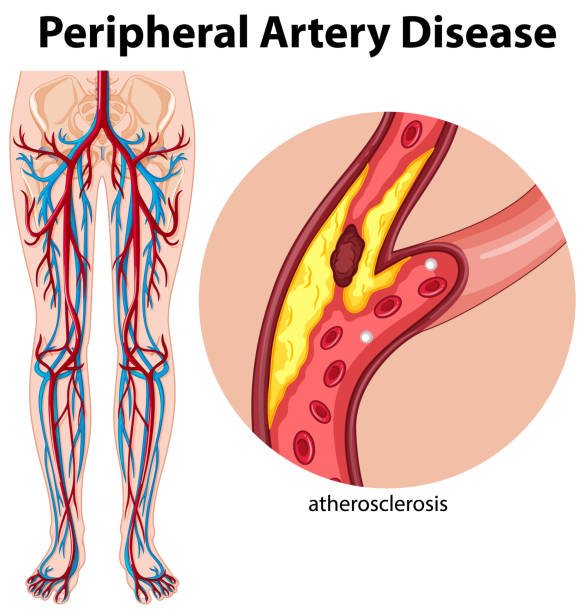
What is peripheral arterial occlusive disease?
Peripheral arterial occlusive disease (PAOD) is the main manifestation of systemic atherosclerosis. Like coronary artery disease and cerebrovascular disease, it is the main cause of death and mobility in patients over 50 years old; as age increases , and its prevalence also increases.
Peripheral artery disease refers to blood circulation problems that occur in arteries other than the coronary arteries, brain arteries, and aortic arch. Generally speaking, tissue ischemia caused by peripheral arterial disease mostly occurs in the lower limbs. The common symptom is ischemic pain, especially around the calf. The most commonly complained symptoms include intermittent claudication and rest in the lower limbs. Restpain, cramping, or coldness. .
Due to diet, high-fat, high-sugar, and high-calorie choices not only lead to nutritional imbalance, but also add risk factors such as diabetes, hypertension, and hyperlipidemia, causing the incidence of peripheral arterial occlusion disease to rise rapidly.

What causes arterial blockage?
Generally speaking, the cause of peripheral artery blockage mostly comes from atherosclerosis, which is the accumulation of fat masses in blood vessels, making the blood vessels narrow or even blocked. It not only causes blockage of peripheral arteries, but also causes blockage of peripheral arteries. It is also the main cause of coronary heart disease.
In rare cases, it may develop due to inflammation of blood vessels, injuries to limbs, abnormal ligament or muscle structure, or even exposure to radiation.
Peripheral arterial occlusive disease symptoms
Many patients with mild symptoms of peripheral arteries rarely experience any symptoms, while symptomatic patients often experience intermittent claudication. Since peripheral artery occlusion often occurs in the lower limbs, patients may experience claudication in their lower limbs when walking or exercising. Pain occurs due to arterial occlusion, but this temporary symptom usually improves after the patient rests for a few minutes. However, if the symptoms of peripheral arterial occlusion worsen, the patient may experience pain even while resting or sleeping. .
Other possible symptoms include:
- Leg numbness and weakness
- Continuous soreness in toes, soles of feet, and legs
- Changes in color of skin on legs
- One leg (foot) becomes cold
- Erectile dysfunction
- Not being able to feel a pulse in your legs or soles of your feet
- Leg skin looks shiny
- Toenails grow slowly
- Leg (foot) hair falls out or grows slowly
Peripheral artery disease grading
Clinically, the manifestations of peripheral arterial occlusive disease can be distinguished in the following four grades:
- Asymptomatic patients: Patients are basically asymptomatic. Upon examination, it may be found that the limbs are easily cold, the peripheral arterial pulse is weakening, or there is a murmur.
- intermittent claudication
- Mild claudication: Intermittent claudication begins after walking 200 steps.
- Moderate to severe claudication: Intermittent claudication after walking less than 200 steps.
- Mild claudication: Intermittent claudication begins after walking 200 steps.
- Pain at rest: Pain may also be felt when resting or sleeping.
- Ulcer or gangrene
When should patients with peripheral artery obstruction seek medical attention?
When you feel numbness or pain in your legs (feet), you can consider seeking medical treatment. Unless you have just crossed your legs or crossed your legs for too long, do not treat it as a natural degeneration of the legs as you age and delay treatment. In addition, even if no symptoms occur, the following patients should seek medical examination:
- Over 65 years old
- Diabetics or smokers over 50 years old
- High-risk groups (obesity, hypertension, etc.)
7 major risk factors for peripheral arterial occlusive disease
Basically, the risk factors for peripheral arterial blockage are very similar to the causes of atherosclerosis:
- High cholesterol
- Hypertension
- Family history (peripheral artery blockage, stroke, heart disease)
- Smokes
- Diabetes
- Older age (those over 50 are at higher risk)
- Too much homocysteine
Four high-risk complications of peripheral arterial occlusive disease
- Critical limb ischemia:
As the arterial blockage becomes severe and turns into chronic limb ischemia, the patient may develop gangrene due to limb injury or infection, and may even require amputation to save life. - Acute limb ischemia:
Acute symptoms of complete occlusion of blood vessels due to blood clots, embolism or trauma. It usually occurs in the lower limbs, which is commonly known as “foot stroke” and requires immediate treatment. In terms of clinical manifestations, there are 6 Ps that can represent: Pain, Paralysis, Parethesia, Pulselessness, Pallor, and Perishing with cold. - Stroke or myocardial infarction:
People with peripheral arterial obstruction may also have fat accumulation in the coronary arteries and carotid arteries. Once they rupture, they may cause acute symptoms of stroke or myocardial infarction. - Serious infection:
If you have a sore or ulcer on your foot that has not healed for a long time, further infection may occur, allowing bacteria to spread to the person’s muscles, bones, or bloodstream.
How is peripheral arterial occlusive disease diagnosed?
Usually, doctors will ask the patient to self-report his symptoms, and then conduct physical examination to find out whether the patient has symptoms such as weakened pulse, blood flow murmur, lowered blood pressure, abnormal skin color, cold skin and other symptoms in the affected area. Other further inspection methods include:
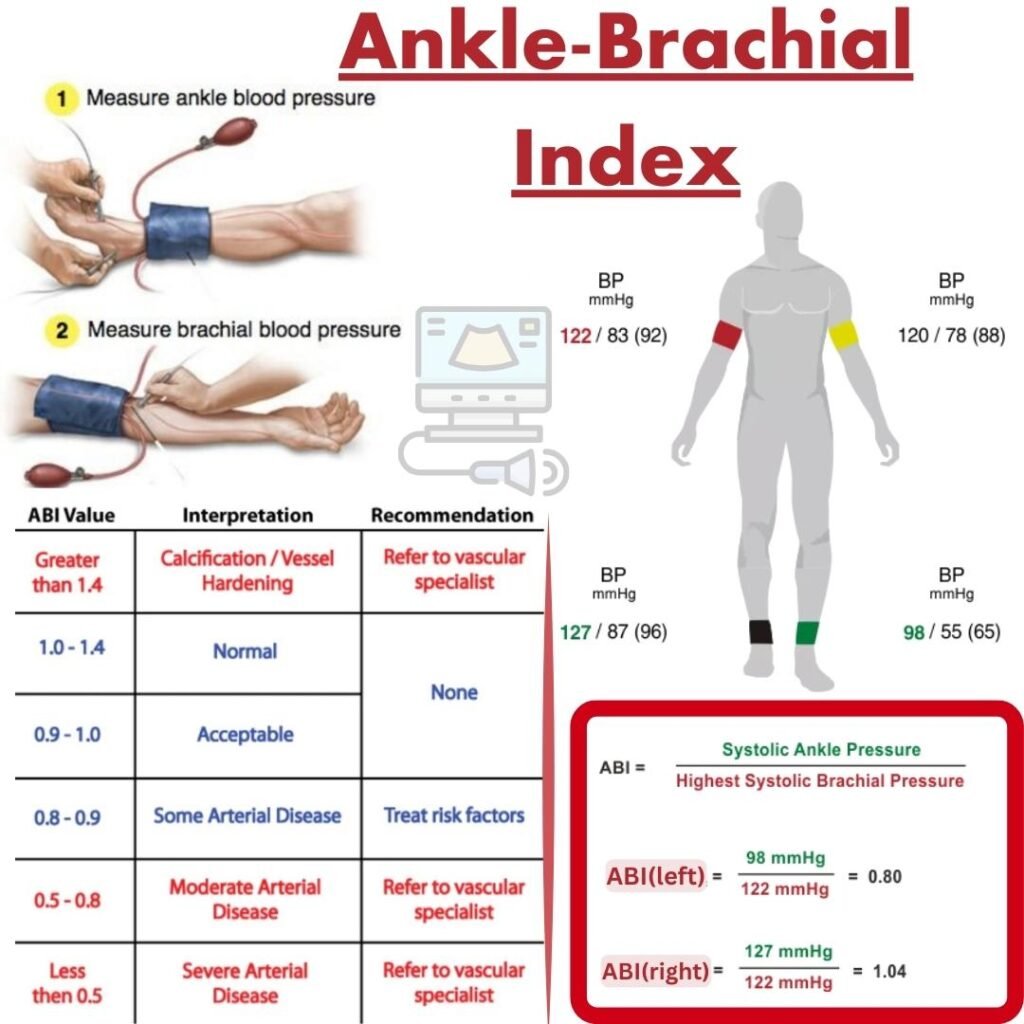
- Ankle Brachial Pressure Index (ABI or ABPI):
Also known as the blood pressure ratio of the upper and lower limbs, it is a common method for detecting peripheral arterial occlusive disease. The doctor will measure the patient’s blood pressure at the ankle and arm. If the blood pressure at the ankle is low, it means the patient may have peripheral artery blockage. - Doppler ultrasound:
Also known as color ultrasound, it can image the blocked arteries. - Angiography:
This is actually the commonly heard cardiac catheterization, but it can also be used to examine parts other than the heart. Usually, a catheter is inserted from the patient’s femoral artery, moved to the area to be examined, and a contrast agent is injected, and used with X-rays to see if there is any blockage in the blood vessel. - Blood test:
Check whether the patient’s triglyceride and cholesterol index are too high.
Peripheral artery occlusive disease treatment methods
Improving patient discomfort and preventing the progression of atherosclerosis are the two main focuses of treatment. Depending on the severity of the patient’s peripheral artery blockage, doctors will consider treatment with exercise training, drugs, or surgery.
- Sports Training
For patients with mild symptoms, doctors may recommend exercise training to improve arterial blood flow and intermittent claudication. This exercise program may be performed in a hospital or on your own, please discuss with your doctor. - Medical treatment
- Cholesterol-lowering drugs: Such as statins, which lower the concentration of bad cholesterol (low-density lipoprotein, LDL) in the body.
- Blood pressure lowering drugs: such as β-blockers, Angiotensin-Converting Enzyme Inhibitors (ACEI)
- Antiplatelet drugs: such as aspirin and cilostazole, which can prevent blood clots from forming and reduce the risk of stroke or myocardial infarction.
- Thrombolytic therapy: Inject drugs into a vein to dissolve blood clots.
- Cholesterol-lowering drugs: Such as statins, which lower the concentration of bad cholesterol (low-density lipoprotein, LDL) in the body.
- Surgical treatment
- Angioplasty: Also called balloon dilatation. Usually, a catheter is inserted from the patient’s femoral artery and guided to the blocked artery. The balloon is inflated to open the blood vessel and increase blood flow. The doctor may decide whether to insert a stent depending on the situation to prevent the blood vessel from becoming narrowed again.
- Bypass surgery: Taking the leg as an example, the doctor will cut off a small section of the leg vein or use an artificial blood vessel for transplantation to replace the originally blocked artery, allowing blood to pass smoothly.
- Catheter-directed thrombolysis (CDT): insert a catheter into the thrombus and inject thrombolytic drugs directly. If the effect is not good, Pharmacomechanical catheter-directed thrombolysis (PCDT) may be used to crush the thrombus with a device, extract the fragments and use thrombolytic agents for treatment.
- Amputation: If the patient’s blockage cannot be treated with medication or surgery, or if the results are ineffective, amputation of the limb with blocked arteries may be considered.
- Angioplasty: Also called balloon dilatation. Usually, a catheter is inserted from the patient’s femoral artery and guided to the blocked artery. The balloon is inflated to open the blood vessel and increase blood flow. The doctor may decide whether to insert a stent depending on the situation to prevent the blood vessel from becoming narrowed again.
How to prevent peripheral arterial occlusive disease?
The best way to prevent peripheral artery blockage is to maintain a healthy lifestyle. The following suggestions are recommended:
- Quit smoking
- Avoid diets high in saturated fat
- Regular exercise
- Diabetic patients should pay attention to blood sugar control to avoid accelerating arteriosclerosis, and it is difficult for diabetic wounds to heal. If there is a wound on the leg without knowing it, it can easily lead to serious infection.












