
What to Do if There is a Septal Defect in the Ventricle? There are 4 Types of Ventricular Septal Defects in Newborns
Ventricular septal defect, as the name suggests, means there is a hole between the left ventricle and the right ventricle. It is the most common congenital heart disease, accounting for about 25 to 30% of all congenital heart diseases. Among children with ventricular septal defects, some neoplasms Children heal before the age of 2 years. Different types of ventricular septal defects have very different chances of natural healing; some ventricular septal defects with large defects may lead to heart failure and may even be life-threatening.
We will take you to understand what a ventricular septum defect is, as well as the types, causes and treatments of a ventricular septum defect.
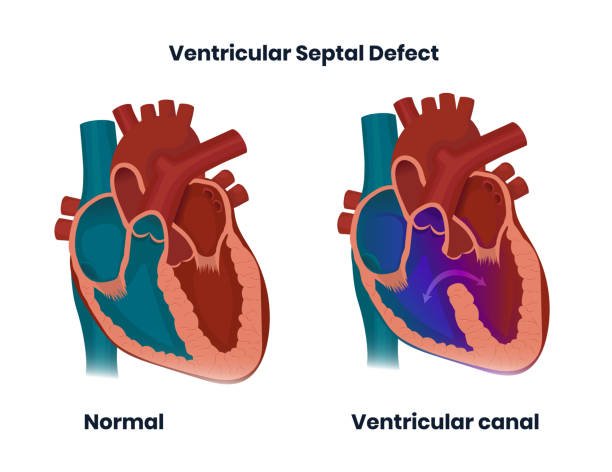
What is a ventricular septal defect?
The human heart has a total of 4 chambers, the left and right atria are on the top, and the left and right ventricles are on the bottom. The body’s used blood flows through the superior vena cava to the right atrium and right ventricle, and is sent to the lungs through the pulmonary artery to obtain oxygen and remove carbon dioxide and waste products; fresh blood rich in oxygen is transported to the left atrium and left ventricle through the pulmonary veins .
If there is a defect in the wall that separates the left and right ventricles of the heart, it is called a “Ventricular Septal Defect (VSD)”. A defect in the ventricular septum can cause blood from the left ventricle to flow from the hole to the right ventricle, causing the following problems:
- Decreased blood flow from the left ventricle to the aorta
- The load on the right ventricle increases, and the amount of blood flowing to the pulmonary artery and lungs also increases
Causes of ventricular septal defect
Studies believe that ventricular middiaphragm defects are mainly caused by the lack of tightness of the middiaphragm muscles during development, and most of them are sporadic problems.
There are 4 types of ventricular septal defects
Depending on the location of the defect, ventricular middiaphragm defects can be divided into 4 types, with different healing rates and complications:
- Type 1: It is more common in Asians. The proportion of diaphragm defects in the ventricle reaches 30%. The hole is located below the aortic valve and pulmonary valve. It is difficult to heal and can easily cause aortic valve prolapse and deformation.
- Type 2: Also known as the membranous type, accounting for about 50-70%, it is the most common ventricular septal defect and may become smaller or heal on its own.
- Type 3: Also known as the atrioventricular cavity type, it is relatively rare, about 5 to 8%, and may be combined with other genetic problems.
- Type 4: also known as muscle type, has a high self-healing rate and accounts for approximately 5 to 20% of ventricular mid-diaphragmatic defects.
Symptoms of ventricular septal defect
Symptoms of septal defect in the ventricle depend on the size of the defect. If the defect is small, only a small amount of blood flows from the left ventricle to the right ventricle. Newborns usually have no special symptoms and can only hear a heart murmur; but if the defect is large, a large amount of blood flows. Shunting can cause the following symptoms:
- Slow growth
- Poor appetite, easy to overflow milk
- Weak crying, restless sleep
- Shortness of breath
- Night sweats, cold limbs
- Hard stool
- Prone to respiratory infections
- Rapid heartbeat
- Enlarged heart
When the diaphragm defect in the ventricle is severe, severe congestion in the lungs can lead to pulmonary hypertension, causing symptoms such as wheezing and cyanosis, and ultimately heart failure.
Diagnosis and treatment of ventricular middiaphragmatic defects
Before treatment, the doctor will first understand the size and location of the defect, the condition of the heart, and whether there is a tendency for the pressure in the right heart and pulmonary artery to increase through the following methods:
Main diagnostic tools
- cardiac ultrasound
Auxiliary inspection
- Electrocardiogram
- Chest X-ray
- Computerized tomography
- Cardiac catheter
- MRI
If the defect is small and has little impact on the heart, the doctor will arrange regular follow-up visits to confirm whether the defect heals on its own. If the defect is serious, medications such as cardiotonic agents (digitales), diuretics or vasodilators will need to be taken; if the defect still cannot be controlled by medication, Or if it has developed into severe pulmonary hypertension, aortic deformation or heart failure, the sick child needs to undergo cardiac catheterization or open heart surgery to correct the problem quickly and avoid life-threatening consequences.












