
The Triangle of Diabetes Management
What is triangle of diabetes management. Let’s study carefully with the following article. The HbA1c test is a tried-and-true way to see how well your glucose levels are controlled. However, a recent study found that the HbA1c measurement should not be considered alone. When attempting to improve your diabetes management, the simplified notion that “lower the HbA1c the better” should arguably not be your primary focus. By focusing solely on lowering your HbA1c, you run the risk of negatively affecting other aspects of your diabetes, increasing the likelihood of hypoglycemic events and swings between high and low glucose levels.
We want to help you understand how this new method can help you get the most out of your FreeStyle meter and improve your diabetes management. Because there is now clear evidence that better management of three goals will lead to improved outcomes, this new concept of the Triangle of Diabetes Care looks at three distinct aspects of your glucose management. When applying the principles of the Triangle of Diabetes Care, even if you only make significant improvements to two of the triangle’s corners, your overall health will benefit, which is positive.
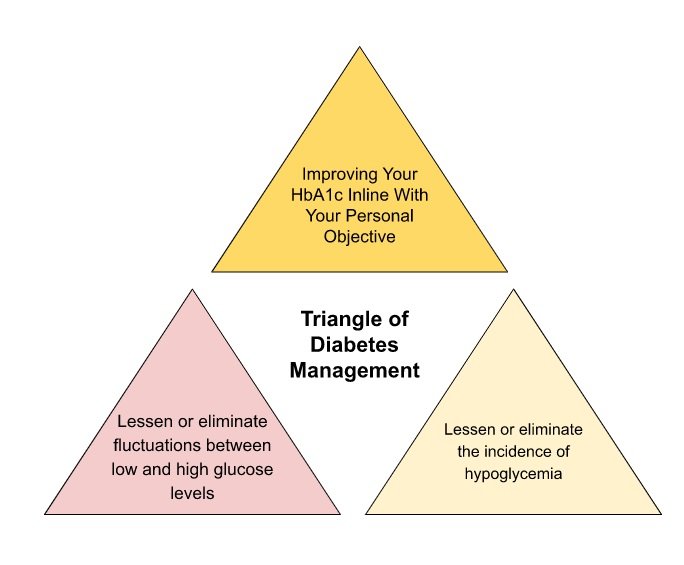
Therefore, what are the three parts of the “Triangle of Diabetes Management”?
- Improve your HbA1c in line with your personal objectives.
- Lessen or eliminate fluctuations between low and high glucose levels.
- Lessen or eliminate the incidence of hypoglycemia.
Explore The Triangle of Diabetes Care modules to learn more about each corner. When it comes to managing your diabetes, you are not alone. However, you need assistance from others. When performed in accordance with a care plan that you have agreed upon with your healthcare provider, glucose self-monitoring is most beneficial. Complications cannot be avoided through testing alone. However, it will provide you with the information you need to modify your treatment to achieve your objectives.
You can achieve better glycemic control, prevent hypoglycemia, and empower yourself to achieve your diet and lifestyle goals by having structured consultations with your doctor or nutritionist.
Improve your HbA1c in line with your personal objectives
Numbers are everything in diabetes, but one is probably on your mind more than any other: your HbA1c. When you meet with your doctor or nutritionist, they probably will take a proportion of your HbA1c. Your doctor can get an overall picture of your average blood glucose levels over a period of weeks or months from this number, which is presented in mmol/mol, such as 51 mmol/mol (previously presented in a percentage, such as 6.8%; see the conversion table for more information). Your individual target goal level of HbA1c will be discussed and agreed upon with your doctor because it is highly dependent on other aspects of your diabetes management and lifestyle. (Two systems to present you HbA1c DCCT in % and IFCC in mmol/mol):
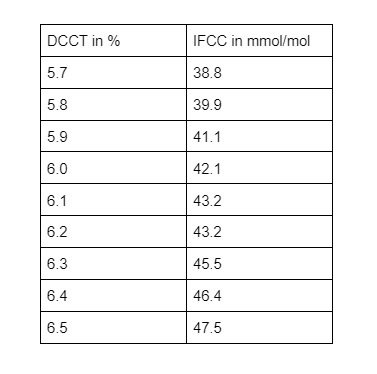
HbA1c is your average blood glucose (sugar) levels for the last two to three months. If you have diabetes, an ideal HbA1c level is 48mmol/mol (6.5%) or below. If you’re at risk of developing type 2 diabetes, your target HbA1c level should be below 42mmol/mol (6%).
It is well established that HbA1c is a marker for understanding glycemic control in type 1 or type 2 diabetes. You will determine a personalized target HbA1c number with your healthcare provider. For instance, if your HbA1c was 48 mmol/mol (6.5 percent), you might be under control, while a figure of 69 mmol/mol (8.5 percent) might tell your doctor that your glucose management needs to be improved. However, if your agreed-upon goal was 58 mmol/mol, a reading of 48 mmol/mol may cause your doctor concern, because it could increase your risk of hypoglycemia episodes.
Recent research has also demonstrated that, despite similar HbA1c levels, patients’ daily glucose patterns can vary significantly. Therefore, keeping accurate records of your daily glucose levels is extremely important. The new scientific guidelines say that if you take insulin via multiple daily injections (MDI), you should test at least four times a day, but up to ten times a day may be necessary in some cases. The reasons for test are as follows:
- Before and snacks.
- After a meal
- Before critical tasks e.g. cycling
- Before exercise.
- When you suspect low blood sugar.
- After treating low blood glucose, such as injection.
- Planning pregnancy, during pregnancy, during breastfeeding.
Scientific guidelines for blood glucose levels include a
- Fasting glucose level of 5-7 mmol/L upon waking.
- Plasma glucose level of 4-7 mmol/L prior to eating.
- After a meal, 5-9 mmol/L
Reducing your HbA1c without properly managing your glucose variability can increase the number of hypoglycemic events, which is a common issue. Numerous diabetics encounter this issue daily. It can be hard to figure out the best way to reduce one factor without increasing the likelihood of hypos.
Hopefully, this clarifies the purpose of the Triangle of Diabetes Care and demonstrates how, rather than focusing solely on your HbA1c goal, working toward the three goals simultaneously will assist in reducing complications in the future.
In this program, the significance of self-monitoring your glucose levels has already been emphasized. You get important direct biological feedback by taking four or more blood glucose readings each day. This may inform you of any necessary behavior adjustments regarding glucose control. This could be accomplished through lifestyle and medication adjustments, which, in the end, may lead to a lower HbA1c.
Lessen or eliminate fluctuations between low and high glucose levels
You are associated with worse outcomes and a high level of glucose variability. Studies indicate that complications increase the risk of death as fasting blood glucose variability rises. It has also been demonstrated that switching from high to low blood glucose increases the risk of cardiovascular disease. Knowledge is power when it comes to effective diabetes management. You will be in a better position to have discussions about how to manage your diabetes, if you know more about it. Building your knowledge is one of the most important reasons to test on a regular basis. This allows you and your doctor to learn about patterns of glucose variability, such as when you go above or below your target range.
Does your blood glucose variation display like the following?

Conducting single-point glucose checks is one of the main reasons why you might have high variability in your glucose levels. In the event that you, take this outcome in segregation, this can prompt you eating to take care of a hypoglycaemic perusing or taking fast acting insulin to diminish a post-feast top. “Catching your blood glucose” is the term for this. You may find that you are chasing your glucose immediately in response to a single reading if you show frequent low and high readings.
A much better strategy involves you and your doctor learning to recognize patterns in your daily glucose levels. On the off chance that you routinely run short or high at explicit seasons of day in light of exercises, these can then be recognized and all the more effectively anticipated. You can discuss how to better manage these predictable trends and guide treatment decisions to improve glucose control as a result of this. For instance, better timing of bites or changing insulin infusions.
Adults with type 1 diabetes could significantly reduce their risk of long-term complications by maintaining near normal glycemia, according to the evidence3. Continuous proficiency in glucose monitoring, insulin dose adjustment, injection technique, and site management are necessary for effective blood glucose control in the current methods. If you want to learn more about management from the NHS, talk to your doctor about taking courses.
The anxiety toward expanded hypos and weight gain can be huge snags to your prosperity, as is squeezing diabetes self-administration into a bustling way of life. Everybody struggles to achieve goals, and some people will succeed more than others. It might be hard to find the time at first, but once you get into a routine, it will be much easier.
I comprehend the idea of glucose variation, but how will this help me?
- Improve your comprehension of and control over your own glucose levels.
- Manage the factors that affect glucose control, such as diet and exercise, by identifying them.
- Adapt to out-of-the-ordinary circumstances like vacations or business trips
- Avoid “chasing your glucose,” which typically results in erratic fluctuations in blood glucose levels.
If you test and record your glucose several times a day, patterns in the fluctuations of your glucose are easier to see. From that information, you and your doctor can then analyze the data and adjust your management schedule.
Pre- and post-meal readings, for instance, will help determine if there is a predictable pattern of glucose change. If this can be identified, it can be managed by reducing your intake of carbohydrates or adjusting the dosage and timing of medications like insulin.
5 steps to help you and your healthcare professional identify glucose trends
- Discuss your blood glucose goals with your doctor in detail.
- Perceive testing designs in your glucose checking diary, and features to examine.
- Talk to your doctor about any circumstances that might be contributing to the erratic trends.
- Examine any potential contribution to glucose trends.
- Reach an agreement on potential solutions that are tailored to your requirements.
This is not going to be a quick fix, and you need to be motivated and supported by your glucose monitoring technology, as well as your doctor.
Shopping “Abbott FreeStyle Libre 2” Online
Keep in mind that prior to meeting with your doctor, simply keeping a detailed diary or downloading and printing reports from our software will allow you to talk about how to fix things for longer and make the consultation 100 percent more valuable. You and your healthcare provider will be able to make the best decisions regarding your diabetes management plan with the assistance of accurate diary records.
Lessen or eliminate the incidence of hypoglycemia
You are sweating profusely, having trouble concentrating, your heart is beating quickly, your mood has changed, and you are feeling sleepy. Are you experiencing hypo? Should you eat something that has a lot of sugar? Simply based on how you feel, it can be difficult to determine when a hypoglycemic event has occurred. One of the three objectives of the Triangle of Diabetes Care is to reduce the number of hypoglycemic episodes.
Your blood glucose level is considered to be “officially” hypoglycemia when it reaches or falls below 3.9 mmol/L2. At this point, you may or may not be experiencing symptoms. Due to the fact that the glucose threshold at which symptoms appear can vary from person to person and even from day to day, it is difficult to establish the threshold for hypoglycemia; You might experience symptoms at various levels.
If you take too much insulin or don’t eat enough, you might have low blood glucose. Since hypoglycemia symptoms vary from person to person, you should try to learn to recognize your own symptoms in order to treat the condition as soon as possible. By testing your glucose on a regular basis, you will get used to recognizing the symptoms of low glucose.
A hypo is never a good time, and it can be frustrating when one strikes without warning or when you treat one only to find that it raises blood glucose much too much. However, it is worthwhile to control hypos not only to avoid disrupting your days or nights but also to improve your glucose control and overall health and wellbeing.
It is very important to be aware of hypoglycemia, but over time you may become less aware, especially if you have long periods of low glucose levels. This is more commonly referred to as “hypo unawareness.” Impaired awareness of hypoglycemia exposes individuals taking insulin, glinides, or sulphonylureas to sudden and unexpected deteriorations of conscious level and unusual behavior, such as slurred speech or clumsiness. It also raises your risk of severe hypoglycemia, which can result in a coma and the potential for death, making it extremely serious. Do not ignore persistent low glucose levels; instead, have it checked by a medical professional.
The number of hypoglycemic events that individuals with type 1 and type 2 diabetes may experience annually is significantly different. A 2004 study looked at self-reported hypoglycemia and found that people with type 1 diabetes were more likely to experience 43 hypoglycemic events per year than people with type 2 diabetes, who were less likely to experience 16 events per year. On the other hand, severe hypoglycemia was uncommon but more common than had previously been shown.
Reduced awareness of hypoglycemia and severe hypoglycemia will make it difficult to do many things you do every day and can put you, your friends, and family through a lot of stress. Additionally, severe hypoglycemia can make you so afraid of having an episode that you won’t be able to meet your glucose goals.
You might find that you have a higher risk of having more hypos if you do a really good job of lowering your HbA1c. Improve your glucose variability and reduce the frequency with which you fluctuate between high and low glucose levels to prevent this from happening. The treatment of diabetes is frequently compared to walking a tightrope—balancing the benefits of ideal glycaemic control with the risks of hypoglycemia to a minimum.5 Another thing to keep an eye out for is the fact that some of the symptoms of low glucose are the same as those of high glucose. Therefore, test whenever you experience symptoms to ensure that you are appropriately treating your glucose level and are not missing a hypo.
- Dizziness
- Blurry vision
- Feeling hungry
- Sweating
- Feeling shaky












