
What is Extracorporeal Membrane Oxygenation? The Principles, Uses, Risks, and Costs of ECMO
Extracorporeal Membrane Oxygenation (ECMO) may be a medical device. Because it is often used in medical conditions involving life and death, some people may have the misconception that using Ye Ke Membrane can prolong life. However, there are actually many conditions and risks that need to be clarified.
This article will introduce the mechanism of action, risks, usage, and health insurance payment conditions of ECMO.
What is ECMO?
In the past, ECMO was mainly used to support heart transplant patients in the transitional period before receiving a heart transplant, or if they did not recover immediately after the heart transplant, ECMO could be used to temporarily replace the heart’s function. However, with the proficiency and popularization of technology, ECMO has now been widely used for patients who require short-term cardiopulmonary function support.
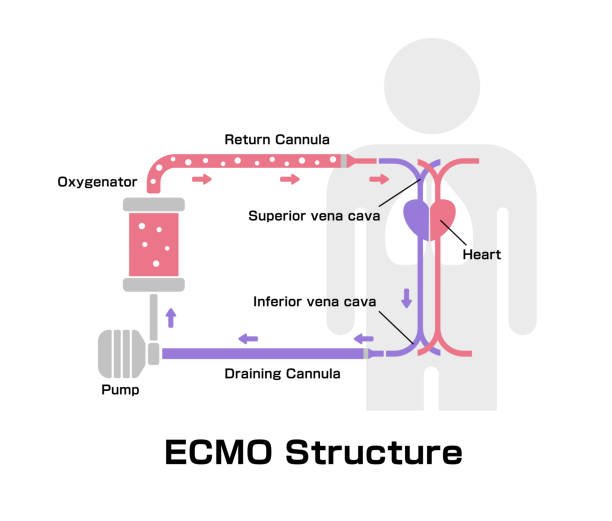
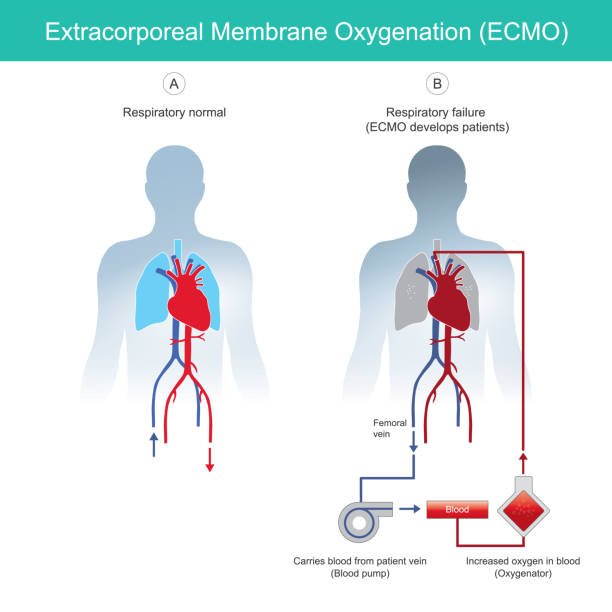
ECMO (also known as extracorporeal membrane oxygenation, extracorporeal circulation membrane lung life support system). The main function is to use an artificial heart (pump) to draw the patient’s blood from the veins, and then use the artificial lung (oxygenator) to remove carbon dioxide from the hypoxic blood, add oxygen to convert it into oxygenated blood, and then convert the blood into oxygenated blood. Infused back into the patient’s artery or vein.
The difference between ECMO membrane and artificial heart-lung machine
Are you smart enough to think that the machine (artificial heart-lung machine) responsible for replacing the heart function during cardiac arrest surgery (Cardiopulmonary bypass) is actually related to ECMO?
Yes, their principles are roughly the same. The artificial heart-lung machine used in cardiac arrest surgery generally only lasts for a few hours until the end of the operation, while the ECMO is used to maintain cardiopulmonary function for days or even weeks.
In addition, the biggest difference between the artificial heart-lung machine and ECMO is whether the blood is stagnant. The artificial heart-lung machine is an open system and can inhale a lot of air during surgery. Therefore, the blood needs to be discharged into a blood storage tank outside the body to remove the air. However, in order to avoid blood coagulation in the blood storage tank, a large amount of anticoagulant must be used. , to avoid thrombosis.
ECMO does not require a blood storage tank, allowing the blood to be in a closed circulation. In addition, the patient’s cardiopulmonary system is not completely disabled, so the blood will not continue to stagnate in one place, so there is no need to use too much of anticoagulant, thereby increasing the usability time of ECMO, allowing extracorporeal circulation to be used outside the operating room.

How to install ECMO?
ECMO membrane needs to be installed through surgery. It mainly consists of a plastic catheter, an artificial lung (oxygenator), and an artificial heart (pump). Medical staff will make a small incision in the patient’s vein or artery to insert the catheter and penetrate it. X-rays are used to confirm that the catheter is in the correct position. At the same time, the patient will be connected to a respirator, so intravenous injection or a nasogastric tube will be used to maintain the patient’s nutritional supply.
In addition, medical staff will also inject anticoagulants to prevent the induced blood from clotting, inject prophylactic antibiotics, and inject sedatives to prevent the patient from becoming agitated. Or diuretics may be given to help the kidneys remove water.
After the installation is completed, the cardiopulmonary bypass technician will monitor the patient’s heart rate, blood pressure, and oxygen content through the screen to ensure the patient’s health condition while using the ECMO.
ECMO connection method
Depending on the patient’s symptoms, ECMO can be mainly divided into the following two application modes:
- Veno-Venous (VV):
The output end is inserted into the femoral vein from the groin, and the output end is located in the cervical vein. It is mainly used for patients with impaired lung function but no risk of cardiac arrest. - Veno-Arterial (VA):
The output end is inserted into the femoral vein from the groin, and the output end is located in the femoral artery. It is mainly used for patients with impaired lung function and risk of cardiac arrest.
Who needs to use ECMO?
People who really need to use ECMO must first be diagnosed by a professional doctor. The principles of judgment include the following three points:
- Even with additional oxygen support, the oxygen supply to the lungs remains insufficient.
- Even with the assistance of a respirator, the lungs cannot properly remove carbon dioxide.
- The heart cannot pump enough blood.
Many diseases may cause the above conditions, such as severe lung infection or myocardial infarction. According to the regulations the following situations are indications for ECMO:
1.Psychogenic shock
- Temporary cardiac dysfunction (Stunned heart) occurs after cardiac surgical reconstruction.
- It is used to temporarily replace the heart function in preparation for heart surgery, ventricular assist device or heart transplantation.
- Reversible cardiomyopathy.
- Pulmonary embolism.
- Acute myocardial infarction and psychogenic shock.
- Other psychogenic shock.
2.Respiratory failure
- FiO2: 1.0, PaO2<60 mmHg, reversible causes have been ruled out.
- Hemodynamic instability caused by CO2 retention has been ruled out as a reversible cause.
- When used as a lung transplant, it is used to temporarily replace lung function.
3.Children and newborns
- Meconium aspiration syndrome
- Respiratory distress syndrome (Hyaline membrane disease)
- Congenital diaphragm hernia (CDH)
- Persistent pulmonary hypertension of neonate (PPHN)
- The above diseases have been treated traditionally (including respirators) and meet the following respiratory failure index:
Oxygenation Index (OI) ≧ 40 OI=MAPxFiO2x100/PaO2
Mean Airway Pressure (MAP)
AaDO2=(Patm–47) x FiO2–PaO2–PaCO2>610 for 8Hrs or >600 for 12Hrs
PaO2<40mmHg for 2hrs
4.Others
- airway trauma
- Extremely hypothermic (core body temperature ≤30°C)
ECMO is not a panacea and is mainly used to maintain cardiopulmonary function.
Affected by media propaganda, Ye Ke film has become a medical device that can be used in critical moments in some people’s minds. However, Ye Ke film itself does not have a “healing” effect, but “temporarily maintains the patient’s cardiopulmonary function.” ”.
If the patient’s condition is serious and cannot be treated, using Ye Keme can only slightly extend the patient’s survival time, but cannot reverse the condition. This is why contraindications must be set to reduce unnecessary waste of health care resources.
All in all, most of the conditions that doctors judge to require the use of Ye Keme are in compliance with the health insurance payment regulations, but there are still some items that the public needs to pay for themselves.
5 major risks of using ECMO
Even if the Ye Ke membrane can provide considerable help to patients with cardiopulmonary incompetence, there are still many inconveniences in using the Ye Ke membrane. For example, patients with Ye Ke membrane cannot move around at will, because any turning over may cause them to collapse. Loose catheters can cause heavy bleeding and may require sedation and immobilization of the hands and feet, but may also increase the risk of pneumonia.
Other risks of using ECMO are as follows:
- Bleeding:
In order to avoid blood coagulation, patients may need to inject heparin. However, the longer ECMO is used, the greater the chance of blood coagulation and other problems occurring. However, long-term use of ECMO membrane and blood anticoagulants may also increase the patient’s bleeding, or destroy blood cells and cause hemolysis. - Kidney failure:
The lack of blood circulation in the kidneys of some patients using ECMO may cause kidney failure. In this case, a machine may be needed to replace kidney function, which is the so-called hemodialysis. - Infection:
Intubation increases the risk of bacteria entering the bloodstream and causing infection in the patient. When the patient is already quite weak, infection may cause the patient’s organ failure and increase the fatality rate. Therefore, doctors may use antibiotics for preventive medication. - Lack of blood supply to the legs:
The blood circulation at the end is extremely poor, especially in the thighs, because the blood is led from the femoral vein to the membrane of the yoke, so the thigh at the cannulation site easily starts to turn black from the toes due to lack of blood supply, and gradually spreads upward. Severe cases may even require amputation. - Stroke:
A patient may experience an embolism caused by air or a blood clot entering a blood vessel. If this blood clot appears in the blood vessels in the brain, causing insufficient blood supply to the patient’s brain, it may cause a stroke.












